Abstract
Background:
Brazil became the South American epicenter for coronavirus disease (COVID-19) soon after the first case was diagnosed in February 2020 with the highest infection rate occurring in the state of Sao Paulo. COVID-19 is characterized by marked thrombo-inflammation mechanisms, and neutrophil-lymphocyte ratio (NLR) among many clinical and laboratory data, is becoming an inflammatory marker of severity and mortality of COVID-19. We evaluated the serial weekly lymphocyte ratios, which are easily derivable from the routine blood counts, in the survivors and non-survivors of COVID-19 at the Clinical Hospital of University of Campinas (UNICAMP), Campinas, Sao Paulo, Brazil, from time of diagnosis to the 3 rd week of care. This hospital is one of the referral centers for COVID-19 patients in this state.
Methods: In this retrospective study, we reviewed the medical notes of 320 adults hospitalized patients with PCR-confirmed COVID-19 at the Clinical Hospital of UNICAMP, from March 2020 to March 2021. The serial weekly hematological parameters (analyzed using automated counter - XN 9000™, Sysmex, Japan) from the time of diagnosis were analyzed and lymphocytes ratios (neutrophil-lymphocyte, NLR, platelet-lymphocyte PLR, and monocyte-lymphocyte MLR) were calculated. The survivors (n=257) were those who recovered from the disease and were discharged from the hospital, while the non-survivors (n=63) were those who died in the course of treatment. Statistical analyses were performed using SPSS (version 22). Unpaired data of Survivors and Non-survivors with COVID-19 were compared using Mann-Whitney tests. Repeated measures were compared within and between groups using univariate and multivariate tests in general linear models. All results were considered significant if p<0.05.
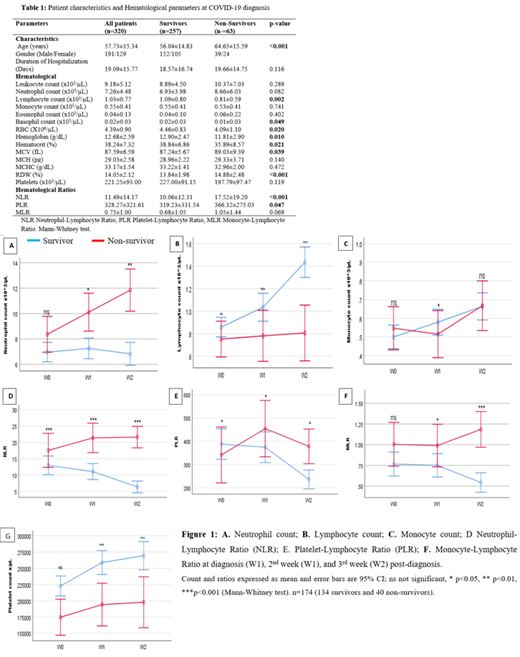
Results: Of the 320 patients, 257 (80.3%) were survivors and had lower mean age than the non-survivors (57.73 vs 64.65 years, p<0.001). At diagnosis, the non-survivors had a lower lymphocyte count (p=0.002), basophil count (p=0.049), and hematocrit (p=0.021) than the survivors, Table 1.
We used general linear models for repeated measures and corrected for the patients who did not stay long enough to have a complete series of blood counts, Figure 1 A-G. Multivariate tests between the survivor and non-survivor groups showed significant variations with serial weekly lymphocyte count (p<0.001), neutrophil count (P=0.005), NLR (p=0.009), MLR (p=0.010), and PLR (p=0.035) but not with the weekly monocyte count (p=0.352) and platelet count (p=0.505). The NLR was higher and PLR was lower in the non-survivors at diagnosis (p<0.001 and p=0.047 respectively), both were higher in the 2 nd week post-diagnosis (p<0.001 and 0.043 respectively), and in the 3 rd week (p<0.001 and p=0.043 respectively) (Figure 1D and E). The MLR was not significantly different at diagnosis but became elevated in the following two weeks post-diagnosis (p=0.09, p=0.022, and p<0.001 respectively) (Figure 1F).
Conclusions: The non-survivors were older and their NLR and MLR tend to increase from the time of diagnosis while their PLR tend to decrease after the 2 nd week post-COVID-19 diagnosis and treatment. On the other hand, all three ratios significantly decrease in the survivors. While neutrophilia and lymphopenia improved in the survivor, they worsen in non-survivors. These cells may have contributed towards the recovery by ameliorating the inflammatory response in survivors, and death by worsening the response in non-survivors of COVID-19. This study shows that serial lymphocyte count, neutrophil count, NLR, PLR, and MLR could serve as good and easily accessible markers of outcomes in patients with COVID-19 and could be used for monitoring of response to treatment.
Costa: Novartis: Consultancy.